|
Pennsylvania Department of Health SWAIM HEALTH CENTER Patient Care Inspection Results |
|
Note: If you need to change the font size, click the "View" menu at the top of the page, place the mouse over the "Text Size" menu item, and select the desired font size. Severity Designations |
| Minimal Citation - No Harm | Minimal Harm | Actual Harm | Serious Harm |
There are 95 surveys for this facility. Please select a date to view the survey results.
|
Surveys don't appear on this website until at least 41 days have elapsed since the exit date of the survey. |
|---|
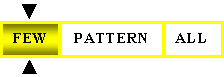
| SWAIM HEALTH CENTER - Inspection Results | Scope of Citation Number of Residents Affected By Deficient Practice |
|